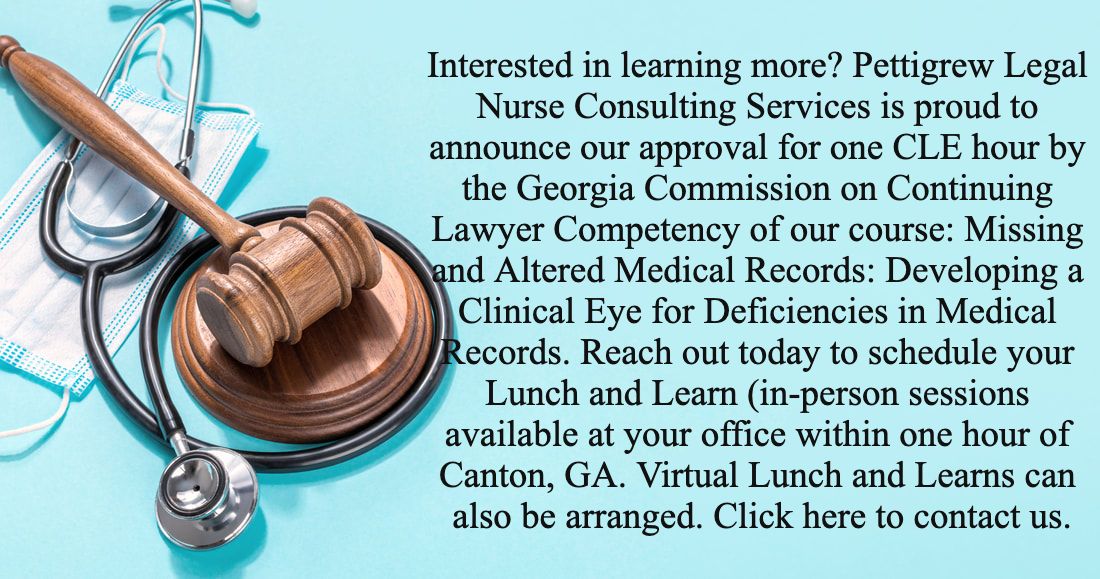
Your law firm is a business; and running a successful business is HARD. There are myriad books, websites, and seminars dedicated to how to run your business, but there are some common threads. According to Forbes Magazine one of the most important steps you can take to run a successful business is to optimize your efficiency by outsourcing what you can.[i] Not a social media guru? Hire a virtual social media pro. Struggle with keeping track of costs? Hire an accountant or bookkeeper. Unfamiliar with medical lingo, the structure of EMRs, and the standard of care? Hire a medical professional to consult with you. A medical professional can greatly reduce the amount of time spent reviewing medical records just by virtue of understanding the structure and content of medical records on a fundamental level. Medical jargon can be as intimidating as another language and understanding the implications of different procedures, items in a medical history, and medications requires literally years of concentrated study and clinical experience- you don’t have time for that! So, “bring in the professionals!” recommends Business News Daily.[ii] A Legal Nurse Consultant is just that- a medical professional with legal knowledge and/or training who can help distill the most pertinent and relevant facts of the case into various reports to help keep your cases moving.
|
Archives
February 2022
AuthorI'm Jennifer Pettigrew and, true story, I first became interested in Legal Nurse Consulting after my auto insurance company was sued following a car accident in which I was found to be at fault. I wasn't sued until after the statute of limitations was up but an exception was made and the plaintiff alleged that because of being rear-ended he was on pain medications chronically which caused him to develop diabetes and become blind. As a nurse I knew that Diabetic retinopathy cannot develop over the course of just a few years but rather is a complication that develops after several years of untreated or poorly treated diabetes. The case was settled by the insurance company before ever going to court for several million dollars, but from that point on I have been interested in the difference medical professionals could make in legal proceedings.
|
Search by typing & pressing enter














 RSS Feed
RSS Feed